- India Medical Mission 2018 - November 1, 2018
- Sleep Disorders: Sleep Apnea and Upper Stimulation Therapy - August 25, 2015
- The Naked Vocalist Podcast Featuring Dr. Reena Gupta - May 27, 2015
- New Therapy for Sleep Apnea – First Sleep Pacemaker placed in California at Osborne Head and Neck Institute. - December 12, 2014
- Boxer’s Ear: Can your ear explode? - December 12, 2014
- Nose Picking (Rhinotillexis) and Septal Perforations: Why I should stop picking my nose…? - November 24, 2014
- Deviated Septum and Septal Perforation - July 28, 2014
- Hereditary Hemorrhagic Telangiectasia: Nasal Septal Perforation Repair - June 25, 2014
- Dr. Mantle recognized at the Beverly Hills Medical Science Academy Awards - May 8, 2014
- Commonly Misdiagnosed Pathologies: Arteriovenous Malformations - April 9, 2014
The generally inaccessible locations of the salivary glands have traditionally led to challenges in accurate diagnosis and treatment of gland pathology. Although greatly improved in modern times, clinicians continue to struggle with these diagnostic challenges, leading to occasional misdiagnosis and delay of appropriate treatment.
The salivary glands are prone to a numerous conditions, some of which are difficult to discern from one another on examination. Arteriovenous malformations (AVM), a rare irregular connection between veins and arteries, are commonly misdiagnosed when they occur within the parotid gland. Failure to recognize these lesions can potentially lead to unforeseen consequences and increase the risk of patient injury.
What is an arteriovenous malformation?
An arteriovenous malformation is an irregular, direct, connection between arteries and veins. Normally, arteries and veins are indirectly connected between networks of very small blood vessels called capillaries. The capillaries are important intermediaries that serve to decrease the pressure of blood and to provide a medium for nutrient/waste exchange between the blood and cells. Arteriovenous malformations can occur in any part of the body and are at increased risk of spontaneous bleeding (hemorrhage).
Who is at risk for AVM development?
A large proportion of AVMs are congenital and present during childhood or early adulthood. There are however certain instances where AVMs will present incidentally later in life. In addition, there are also a few hereditary diseases that include an increased risk of AVM formation including, Hereditary Hemorrhagic Telangiectasia and Von Hippel Lindau Disease.
Why are AVMs in the parotid dangerous?
An AVM is a vascular lesion that is particularly unstable because of the direct union of arteries to veins. Due to the high pressure found in arteries, AVMs are prone to leakage and at times severe hemorrhage. When these lesions are not clearly identified preoperatively, surgeons could inadvertently cut them, leading to a potentially life threatening blood loss.
How do I know if I have an AVM?
AVMs are typically asymptomatic and the patient is usually unaware they even have one. These lesions are usually found incidentally during treatment or evaluation of another issue. In other cases AVMs can cause inflammation or physical distortion of the overlying and surrounding tissues prompting their diagnosis. In some cases an AVM occurring in the parotid gland can be confused with salivary gland stones (sialolithiasis), salivary neoplasm or lymphoma.
Why are AVMs misdiagnosed?
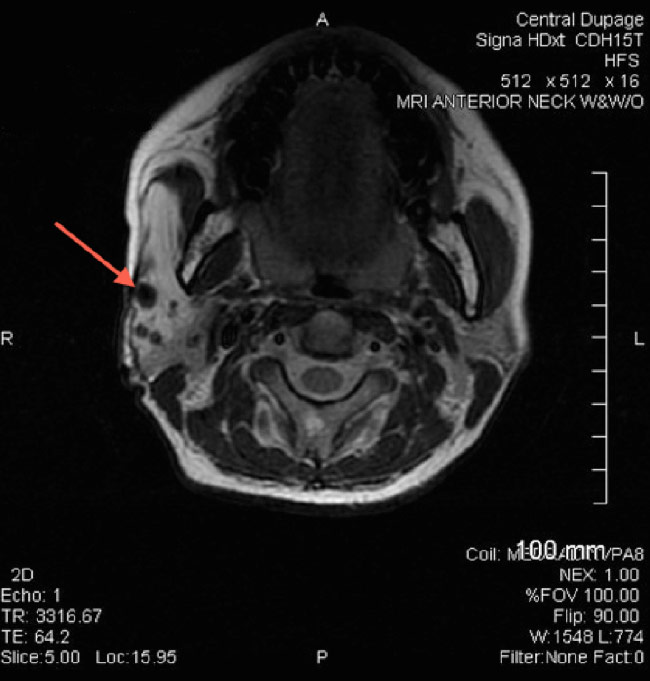
AVMs can develop deep within the salivary glands leading to subsequent external inflammation of the face. On initial external evaluation a physician may confuse this with tumor growth. In addition, traditional imaging studies often cannot adequately discern between AVMs and salivary gland stones (sialolithiasis) or tumor growth. Furthermore, because AVMs tend to be rare, many clinicians have never encountered them, increasing the likelihood of misdiagnosis.
How can I decrease the likelihood of AVM misdiagnosis?
Obtaining proper evaluation by a qualified salivary gland specialist can decrease the likelihood of AVM misdiagnosis. Evaluation of a suspected salivary gland mass typically involves CT or MRI imaging. When insufficient to provide a definitive diagnosis, specialized imaging such as magnetic resonance angiography (MRA) is obtained. During an MRA special contrast material is introduced into the blood vessel to better distinguish vessels on imaging. Together with a thorough clinical history and proper physical examination, the salivary gland specialist can differentiate common salivary gland issues from more subtle and rare issues that require specialized care.
The physicians of the Osborne head and Neck Institute are experts at diagnosis and treatment of both common and rare disorders of the salivary glands. Dr. Ryan Osborne, Director of Head and Neck Surgery at the Osborne Head and Neck Institute, is double board certified in Otolaryngology and Head and Neck Surgery. Dr. Osborne’s decades of clinical experience and unparalleled expertise in salivary gland disorders has resulted in international acclaim and excellent patient outcomes.
Please contact the Osborne Head and Neck Institute to learn more.