- Hereditary Hemorrhagic Telangiectasia - May 25, 2016
- Hereditary Hemorrhagic Telangiectasia: Septal Perforation and Nose Bleeds - May 23, 2016
- Hereditary Hemorrhagic Telangiectasia: Epistaxis and Septal Perforation - May 18, 2016
- Wegener’s Granulomatosis: Autoimmune Disease and Multi-Focal Septal Perforation - May 9, 2016
- Kyle Korver: Facial Injury and Nasal Fracture - March 24, 2015
- Russell Westbrook: Facial Injury and Surgery - March 5, 2015
- Mega-perforation: Pushing the Limits of Septal Perforation Repair - November 26, 2014
- Septoplasty Complication and Septal Perforation - November 24, 2014
- Nose Picking (Rhinotillexis) and Septal Perforations: Why I should stop picking my nose…? - November 24, 2014
- Nasal Fractures, Septal Hematoma, and Septal Perforation: Simultaneous Rhinoplasty and Septal Perforation Repair - October 1, 2014
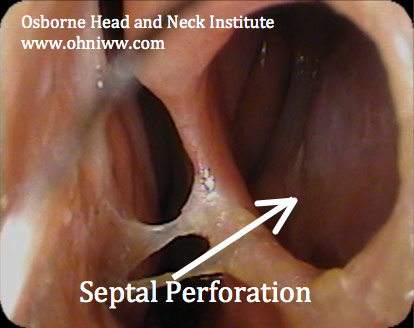
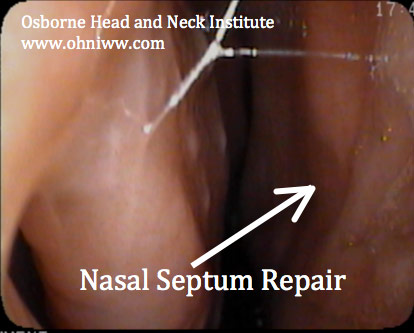
Nasal Septum Repair/Septal Perforation Surgery/Nose Deformity
CLINICAL CHALLENGE
Septal perforation surgery is likely one of the most difficult reconstructive surgical procedures performed by a nasal reconstructive surgeon. Long-term follow-up is mandatory to insure that the perforation heals well without complications.
MANAGEMENT CONSIDERATIONS
The complexity of each case is dictated by the cormorbidities present.
Patients presenting with septal perforations may have a history of nasal fracture, deviated septum, prior surgery, illicit drugs use, allergic rhinitis (hay fever), sinus disease and/or turbinate hypertrophy. Many patients may also suffer from depressive disorders, anxiety, or obsessive complusive disease. Proper management requires managing all factors that could compromise the surgical outcome of the patient. This may require comanagement with an internist, allergy specialist, ENT, and occasionally psychologist/psychiatrist.

CLINICAL RESULTS
Patients are most satisfied when all procedures can be completed in one setting. Rhinoplasty, septoplasty, turbinate reduction, sinus surgery, septal perforation repair, and nasal collapse should all be performed with one procedure. This case presents a patient that underwent correction of a deviated septum, turbinate reduction, and rhinoplasty in conjunction with his septal perforation repair. The results shown are of a one-year follow-up.
SURGEON COMMENTS
Dr. Hamilton- “Recovery from septal perforation surgery is relatively quick in proportion to the degree of difficulty associated with the surgery. Never-the-less, it takes months after the “bandages come off” before the nose feels completely normal inside. This may seem like an eternity to a patient who has suffered with a perforation for years, and may be very anxious regarding the final results. Proper recovery requires a lot of t.l.c. from the physician and lots of patience on the part of the patient, but in the end nearly all patients see positive results from their surgery.”
Dr. Jason Hamilton is the Director of Plastic and Reconstructive Surgery for the Osborne Head and Neck Institute, and is double board certified by the American Board of Facial Plastic and Reconstructive Surgery and the American Board of Otolaryngology/Head and Neck Surgery. Dr. Hamilton is one of only handful of septal perforation specialist worldwide.
Click here to download article PDF
For more information on the deviated septum, septoplasty, functional rhinoplasty, and septal perforation repair by Dr. Jason Hamilton, septal perforation specialist, please contact the Osborne Head and Neck Institute or visit www.perforatedseptum.com.