- What is Vocal Cord Paralysis? - December 15, 2015
- Have You Heard of Wegener’s? - December 15, 2015
- Otitis Externa – Swimmer’s Ear - December 15, 2015
- Hereditary Hemorrhagic Telangiectasia - May 25, 2016
- Hereditary Hemorrhagic Telangiectasia: Septal Perforation and Nose Bleeds - May 23, 2016
- Hereditary Hemorrhagic Telangiectasia: Epistaxis and Septal Perforation - May 18, 2016
- Wegener’s Granulomatosis: Autoimmune Disease and Multi-Focal Septal Perforation - May 9, 2016
- Kyle Korver: Facial Injury and Nasal Fracture - March 24, 2015
- Russell Westbrook: Facial Injury and Surgery - March 5, 2015
- Mega-perforation: Pushing the Limits of Septal Perforation Repair - November 26, 2014
- Septoplasty Complication and Septal Perforation - November 24, 2014
- Nose Picking (Rhinotillexis) and Septal Perforations: Why I should stop picking my nose…? - November 24, 2014
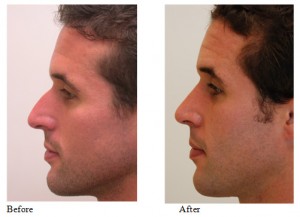
- Nasal Fractures, Septal Hematoma, and Septal Perforation: Simultaneous Rhinoplasty and Septal Perforation Repair - October 1, 2014
Wegener’s Granulomatosis is a fairly uncommon autoimmune disorder in which small arterial blood vessels are attacked by the body, restricting blood flow to various organs. This ultimately results in scar tissue and organ injury.
Autoimmune disorders are conditions in which the body inflicts harm onto itself, thinking the targeted area is harmful and foreign. Wegener’s Granulomatosis attacks small arterioles, creating a granuloma, a collection of inflammatory cells within a tissue. Wegener’s often targets the small arterial blood vessels located near the kidneys, lungs, ears, and nasal septum. Symptoms vary according to how active the disease is, making it difficult to diagnose at times.
Physicians recognize Wegner’s by identifying any of the following symptoms:
- Runny-nose
- Cough
- Ear infection
- Chest pain
- Bloody cough
- Blood in urine
- Ulceration of the mucous membrane
- Red eyes
- Shortness of breath
- Feeling of weakness
- Fever
There is no defined explanation for the cause of this disorder, or why the body begins to attack the small vessels in these organs. Doctors diagnose Wegener’s by performing various tests and procedures, including: urinalysis, CT Scans, X-rays, and tissue biopsies.
When formulating a treatment plan for Wegener’s Granulomatosis, physicians consider the relative activity of the disease (i.e., active vs. inactive disease). In some cases, this distinction is not readily apparent because tissue inflammation and scarring can be the result of active disease, but it can also be the result of previously-active disease.
If tissue damage is determined to be the result of previously-active disease, immunosuppressive medicine is generally not used. Determining the severity of active and inactive Wegner’s Granulomatosis generally determines the patient’s need for immunosuppressive therapy, tissue grafts, or organ transplants down the line.
When treated early, Wegner’s Granulomatosis patients can experience significant recovery. In contrast, more severe cases or instances in which treatment has been delayed can result in significant disease progression and organ dysfunction.
Wegener’s can result in serious complications:
- Kidney Failure
- Lung Failure
- Hearing Loss
- Breathing Problems
Wegener’s can lead to kidney failure. Crescentic glomerulonephritis, rapid kidney inflammation caused by an immune response, affects about 85% of all Wegner’s cases.
Glomerulonephritis symptoms include:
- High blood pressure
- Foamy or pink urine
- Fatigue
- Swelling in the face
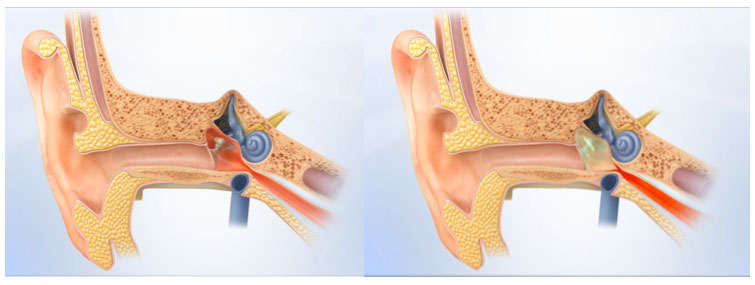
Otologic involvement, such as middle ear infections, is seen in 40-70% of patients diagnosed with Wegener’s Granulomatosis. Eustachian tube dysfunction in these patients may cause a middle ear infection, tympanic perforation, granulation tissue in the ear, and conductive hearing loss from a scarred tympanic membrane. Less commonly seen is vertigo from granulomas or vasculitis in the inner ear. To treat for middle ear infections caused by Wegener’s Granulomatosis, doctors will recommend immunosuppressive drugs and ventilation tubes to drain the middle ear.
The respiratory tract is affected in 93% of Wegener’s Granulomatosis patients. When this occurs in the nasal mucosa, obstruction of the nasal passages may occur. Inflammation can destroy surrounding tissues, leading to septal perforations, saddle nose deformity, and/or nasal pain. The risk of septal perforation is high in these cases and conservative and specialized care should be considered. Treatments may initially include topical antibiotics and saline solution rinses.
Subglottic stenosis, or narrowing of the airway in the larynx, occurs in about 18% of Wegener’s Granulomatosis patients. The patient may experience trouble breathing, hoarseness, and throat irritation. Treatments for this region include advanced airway expansion surgery or tracheotomy to bypass any obstruction. In severe cases of airway compromise, emergent treatment may become necessary.
Despite advances in therapy, tissue damage and medication side effects impact the quality of life of up to one third of Wegner’s patients. If untreated, Wegner’s Granulomatosis patients are at increased risk of death. Any suspected cases of Wegener’s Granulomatosis should be reported to a physician immediately. With treatment, most patients recover and improve within a couple of months. Therapy lasts about two years and may require consistent follow-up care.
Key Facts:
- Wegener’s Granulomatosis is an autoimmune disorder that can affect the lungs, kidneys, ears, and nasal septum
- When treated early, Wegner’s Granulomatosis patients can experience significant recovery
- Severe cases or instances in which treatment has been delayed can result in significant disease progression and organ dysfunction
- Wegener’s can lead to many complications (i.e., renal issues, loss of proper breathing, and changes in hearing)
- Moral support is necessary for patients with Wegener’s Granulomatosis
To learn more about Wegener’s Granulomatosis or Dr. Jason Hamilton, please visit: www.ohni.org.