- Hereditary Hemorrhagic Telangiectasia - May 25, 2016
- Hereditary Hemorrhagic Telangiectasia: Septal Perforation and Nose Bleeds - May 23, 2016
- Hereditary Hemorrhagic Telangiectasia: Epistaxis and Septal Perforation - May 18, 2016
- Wegener’s Granulomatosis: Autoimmune Disease and Multi-Focal Septal Perforation - May 9, 2016
- Kyle Korver: Facial Injury and Nasal Fracture - March 24, 2015
- Russell Westbrook: Facial Injury and Surgery - March 5, 2015
- Mega-perforation: Pushing the Limits of Septal Perforation Repair - November 26, 2014
- Septoplasty Complication and Septal Perforation - November 24, 2014
- Nose Picking (Rhinotillexis) and Septal Perforations: Why I should stop picking my nose…? - November 24, 2014
- Nasal Fractures, Septal Hematoma, and Septal Perforation: Simultaneous Rhinoplasty and Septal Perforation Repair - October 1, 2014
- India Medical Mission 2018 - November 1, 2018
- Sleep Disorders: Sleep Apnea and Upper Stimulation Therapy - August 25, 2015
- The Naked Vocalist Podcast Featuring Dr. Reena Gupta - May 27, 2015
- New Therapy for Sleep Apnea – First Sleep Pacemaker placed in California at Osborne Head and Neck Institute. - December 12, 2014
- Boxer’s Ear: Can your ear explode? - December 12, 2014
- Nose Picking (Rhinotillexis) and Septal Perforations: Why I should stop picking my nose…? - November 24, 2014
- Deviated Septum and Septal Perforation - July 28, 2014
- Hereditary Hemorrhagic Telangiectasia: Nasal Septal Perforation Repair - June 25, 2014
- Dr. Mantle recognized at the Beverly Hills Medical Science Academy Awards - May 8, 2014
- Commonly Misdiagnosed Pathologies: Arteriovenous Malformations - April 9, 2014
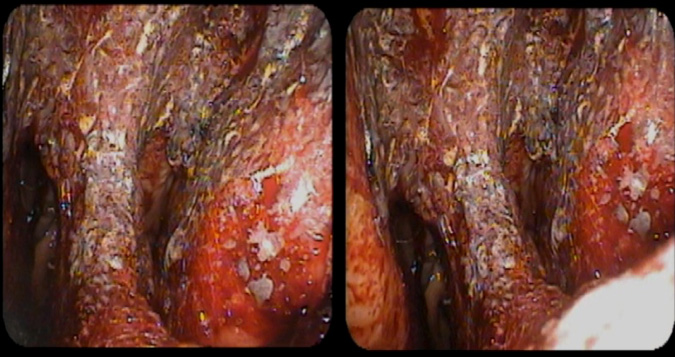
Hereditary Hemorrhagic Telangiectasia (HHT), also known as Osler-Weber-Rendu Disease, is a genetic disease that is characterized by the aberrant overgrowth and proliferation (dysplasia) of vascular tissue known as telangiectasias and arteriovenous malformations (AVMs). Because these newly formed vascular tissues are located at incorrect locations and improperly formed, they are prone to bleeding and in some cases, serious hemorrhage. HHT is highly variable and symptoms and prognosis depend on the severity of the disease’s clinical manifestations.
One of the most common manifestations of HHT is repeated and severe nose bleeds (epistaxis). When telangiectasia form in the nasal passages, repeated drying and trauma from sneezing or nose picking (rhinotillexis) can cause episodes of epistaxis. Traditional treatment of telangiectasias in the nasal cavities involves cautery that burns and seals the causative tissue. Because telangiectasias frequently form on or around the nasal septum, the process of cautery can result in perforation of the septum, leading to a series of nasal issues and potential complications.
Who is at Risk for HHT?
HHT is a rare autosomal dominant genetic disease that is usually seen within families. Because the gene for HHT is “dominant”, families with one parent suffering from HHT, have at least a 50% chance of having a child with HHT. Since HHT is passed from parent to child via genetic inheritance, the disease is not transmissible in any other fashion or contagious. Even though the gene for HHT is dominant, the pattern of disease expression and symptom manifestation can vary considerably even within the same family with some members displaying benign symptomatology and others developing more advanced clinical issues.
What are the symptoms of HHT?
HHT is a highly variable disease that can be clinically silent in some and severely debilitating in others. Milder cases present with repeated cases of nosebleeds, sometimes occurring at night during sleep. More advanced cases can result from arteriovenous malformations occurring within the bodies organ tissues such as the brain, lung, liver, gastrointestinal tract, urinary tract, trunk, and the arms and fingers.
Because nosebleeds are the most common manifestation of HHT, the remainder of this article focuses on the implications of HHT manifestation in the nasal cavities and subsequent complications such as nasal septal perforation.
What are the symptoms of a septal perforation?
Septal perforations can cause repeated episodes of nasal passage drying, crusty and dried mucus, whistling noises during respiration, and possible bleeding. In addition to these symptoms, septal perforations can grow in size over time, compromising the support structure of the nose, leading to depressions in the nose and other undesirable cosmetic changes.
Why should I have my septal perforation repaired?
The function of the nasal septum is to structure and organize the flow of air into the nasal passages. In addition the nasal septum serves to stabilize and support the structure of the nose. Compromise to the structure of the nasal septum can cause not only undesirable cosmetic changes but also result in functional complaints such as nasal obstruction or increased bleeding and dryness.
Who should repair my septal perforation?
Septal perforation repair should only be performed by a highly qualified and experienced surgeon. In the right hands, septal perforation repair and nasal reconstruction have a high success rate. For surgeons who rarely perform the surgery, success rates hover around 30%.
The physicians of the Osborne Head and Neck Institute are board certified in otolaryngology and plastic and reconstructive surgery. These surgeons carry a rare and complimentary subset of training specialties, allowing them to address not only the functional concerns of the nose but also the aesthetic implications of disease treatment.
To learn more about Dr. Jason Hamilton, septal perforation repair, or hereditary hemorrhagic telangiectasia, please visit www.perforatedseptum.com