- Hereditary Hemorrhagic Telangiectasia - May 25, 2016
- Hereditary Hemorrhagic Telangiectasia: Septal Perforation and Nose Bleeds - May 23, 2016
- Hereditary Hemorrhagic Telangiectasia: Epistaxis and Septal Perforation - May 18, 2016
- Wegener’s Granulomatosis: Autoimmune Disease and Multi-Focal Septal Perforation - May 9, 2016
- Kyle Korver: Facial Injury and Nasal Fracture - March 24, 2015
- Russell Westbrook: Facial Injury and Surgery - March 5, 2015
- Mega-perforation: Pushing the Limits of Septal Perforation Repair - November 26, 2014
- Septoplasty Complication and Septal Perforation - November 24, 2014
- Nose Picking (Rhinotillexis) and Septal Perforations: Why I should stop picking my nose…? - November 24, 2014
- Nasal Fractures, Septal Hematoma, and Septal Perforation: Simultaneous Rhinoplasty and Septal Perforation Repair - October 1, 2014
- India Medical Mission 2018 - November 1, 2018
- Sleep Disorders: Sleep Apnea and Upper Stimulation Therapy - August 25, 2015
- The Naked Vocalist Podcast Featuring Dr. Reena Gupta - May 27, 2015
- New Therapy for Sleep Apnea – First Sleep Pacemaker placed in California at Osborne Head and Neck Institute. - December 12, 2014
- Boxer’s Ear: Can your ear explode? - December 12, 2014
- Nose Picking (Rhinotillexis) and Septal Perforations: Why I should stop picking my nose…? - November 24, 2014
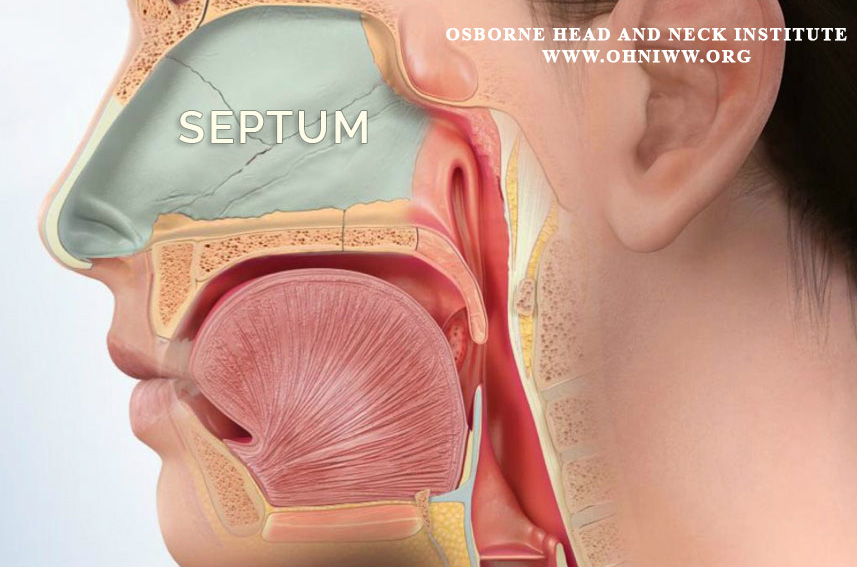
- Deviated Septum and Septal Perforation - July 28, 2014
- Hereditary Hemorrhagic Telangiectasia: Nasal Septal Perforation Repair - June 25, 2014
- Dr. Mantle recognized at the Beverly Hills Medical Science Academy Awards - May 8, 2014
- Commonly Misdiagnosed Pathologies: Arteriovenous Malformations - April 9, 2014
Diagnosis and Treatment of Epistaxis: Preventing Septal Perforations
HHT Overview
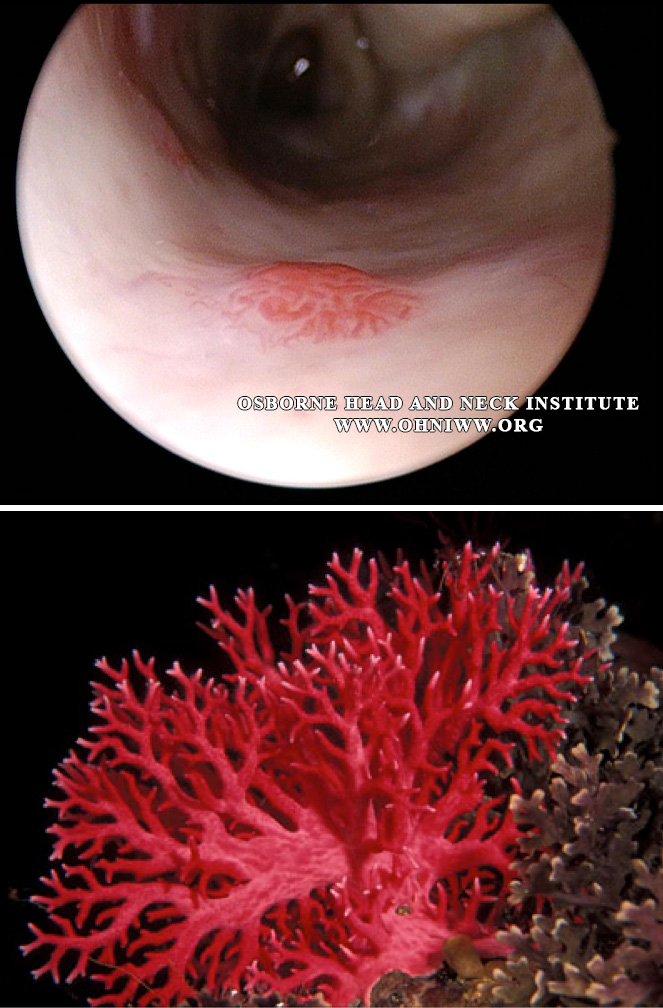
Hereditary Hemorrhagic Telangiectasia (HHT) is a hereditary disorder characterized by abnormal clusters of weak bulging capillaries that bleed with little to no trauma or insult. They most commonly affect the nasal mucosa, but also involve the gut, skin, brain and lungs as well. Clinically patients most commonly report a history of recurrent nosebleeds (epistaxis) before being diagnosed with HHT and may suffer from lifelong recurrent epistaxis that may increase in severity as the patient ages. Epistaxis may be a simple nuisance to the patient or severe bleeding requiring multiple transfusions, hospitalizations and significantly impacting a patient’s work and social life.
Clinical Challenge
Treatment of HHT related epistaxis is often administered when the HHT patient has an acute nosebleed episode and may including nasal packing or cauterization of the acute bleeding site. The problem with this method of cautery is that the bleeding site is poorly visualized in the acutely bloody nose. The ideal setting would include; visualization under magnified endoscopy, a secure airway (intubation, general anesthesia) to prevent blood trickling down the throat and causing coughing during the procedure, and some form of cautery to stop the bleeding. This would typically require the patient to be taken to the operating room, placed under general anesthesia and cautery performed with direct visualization. Even in this scenario the bleeding site is difficult to locate because the patient may have multiple telangiectasias sites within the nose. It may be a “coin toss” to decide which telangiectasia is the culprit in a particular nosebleed episode. If all of the HHT telangiectasia sites are treated at once it may lead comprise of the blood supply to the nasal septum leading to a septal perforation from over-cauterization.
Clinical Considerations
The ideal management protocol for the HHT patient with clinically significant epistaxis would be to treat potential bleeding sites early, between acute episodes of epistaxis, when the telangiectasias can easily visualized and cauterization procedures can be spaced out to allow the nose to recovery between sessions. This helps prevent compromising the blood supply to healthy mucosa and minimizes the risk of septal perforations. Early control of HHT epistaxis may also prevent the need for Young’s procedure or a septal perforation repair surgery, which are much more difficult procedures to perform and has longer recovery times.
Surgeon Comments
Dr. Jason Hamilton, Director of Plastic and Reconstructive Surgery at the Osborne Head and Neck Institute, is double board certified by the American Board of Facial Plastic and Reconstructive Surgery and the American Board of Otolaryngology/Head and Neck Surgery. His extensive training and expertise provide him with a unique perspective to address both functional and aesthetic concerns of the nose.
For more information on hereditary hemorrhagic telangiectasia or septal perforation repair, please contact the Osborne Head and Neck Institute or visit www.perforatedseptum.com.