
- Keloid Treatment Options - September 25, 2017
- Hereditary Hemorrhagic Telangiectasia - May 25, 2016
- Hereditary Hemorrhagic Telangiectasia: Septal Perforation and Nose Bleeds - May 23, 2016
- Hereditary Hemorrhagic Telangiectasia: Epistaxis and Septal Perforation - May 18, 2016
- Wegener’s Granulomatosis: Autoimmune Disease and Multi-Focal Septal Perforation - May 9, 2016
- Kyle Korver: Facial Injury and Nasal Fracture - March 24, 2015
- Russell Westbrook: Facial Injury and Surgery - March 5, 2015
- Mega-perforation: Pushing the Limits of Septal Perforation Repair - November 26, 2014
- Septoplasty Complication and Septal Perforation - November 24, 2014
- Nose Picking (Rhinotillexis) and Septal Perforations: Why I should stop picking my nose…? - November 24, 2014
- Nasal Fractures, Septal Hematoma, and Septal Perforation: Simultaneous Rhinoplasty and Septal Perforation Repair - October 1, 2014
A keloid is a scar that forms due to an overgrowth of collagen, a protein found in skin, at the site of a healing injury. Unlike typical scars, keloids grow beyond the boundaries of their original wounds and do not regress over time. Individuals of African, Hispanic, and Asian descent and individuals between the ages of 10 and 30 are most susceptible to the formation of keloids; however, keloids can develop on anyone regardless of ethnicity and age.
Treatment for keloids includes steroid injection, surgical excision, laser treatment, radiation, and cryotherapy. All cases of keloids should be individually evaluated by a physician to decide what treatment plan is most appropriate.
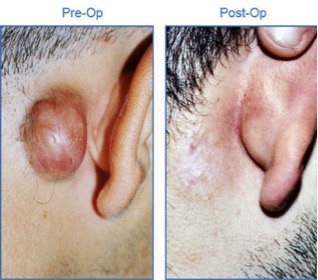
Steroid Injections: Most keloids will respond to injections of a steroid called triamcinolone that reduces the production of collagen and other proteins that form fibrous scar tissue. These injections soften and flatten keloids; however, they must be performed monthly for 3-6 months and rarely eliminate keloids entirely. In order to increase the overall effectiveness of treatment, steroid injections are often administered with an additional form of therapy, such as cryotherapy.
Surgical Excision: Many doctors surgically excise keloids. This treatment has a very high recurrence rate because keloids are formed on incision sites. Excisions require that an incision be made. For this reason, surgical removal is also combined with radiation therapy or steroid injections in order to lower the rate of recurrence after excision.
Laser Treatment: The Pulsed Dye Laser (PDL) uses a concentrated beam of light to destroy the vessels that are supplying blood to the keloid, reducing redness and swelling. This treatment is safe and not very painful; however, multiple treatment sessions may be needed. Patients may avoid laser treatments because of the high cost and the risk of failure to effectively shrink the keloid.
Radiation: Radiation is commonly used to treat keloids that cannot be surgically removed. Radiation permanently destroys existing collagen-producing cells and limits the production of new ones. Internal radiation, brachytherapy, is used for keloids that are linear shaped or in curved areas. External electron beam irradiation is used for large and bulky keloids in a fairly flat area of the body. Although radiation is usually successful, it is typically reserved as a last choice due to the higher risk of causing cancer.
Cryotherapy: Cryotherapy utilizes liquid nitrogen at extremely low temperatures to freeze the keloid. This application destroys keloid tissue from the inside out. Cryotherapy is very effective because after treatment the keloid turns into a scab and gradually shrinks in size until it completely falls off. This mechanism avoids any type of incision and flattens the keloid in its entirety, significantly reducing the rate of recurrence.
The methods listed above work individually or in combination to achieve the patient’s desired outcome. Although cryotherapy is the primary method used at Osborne Head and Neck Institute, not all cases respond to this therapy and patients should be individually examined in order to determine the best treatment plan.
To learn more about keloid treatment, please visit: www.ohni.org.



