- Folded Ear in Newborns: Treatment Options - April 11, 2018
- Newborn Ear Deformity: What Can Be Done? - April 11, 2018
- Ear Molding: An Overview - November 2, 2017
- Otoplasty for Protruding Ears - September 26, 2017
- Basal Cell Carcinoma: Facial Reconstruction Timing - September 26, 2017
- Clinical Considerations of Mohs Reconstruction of Cheek Defect - September 26, 2017
- Basal Cell Carcinoma: Nasal Bridge Reconstruction - September 26, 2017
- Skin Cancers Involving the Eyebrow: Clinical Considerations - October 3, 2016
- Treatment of Multiple Skin Cancer Lesions - June 1, 2016
- Skin Cancer: Nasal Reconstruction and Scar Management - June 1, 2016
- India Medical Mission 2018 - November 1, 2018
- Sleep Disorders: Sleep Apnea and Upper Stimulation Therapy - August 25, 2015
- The Naked Vocalist Podcast Featuring Dr. Reena Gupta - May 27, 2015
- New Therapy for Sleep Apnea – First Sleep Pacemaker placed in California at Osborne Head and Neck Institute. - December 12, 2014
- Boxer’s Ear: Can your ear explode? - December 12, 2014
- Nose Picking (Rhinotillexis) and Septal Perforations: Why I should stop picking my nose…? - November 24, 2014
- Deviated Septum and Septal Perforation - July 28, 2014
- Hereditary Hemorrhagic Telangiectasia: Nasal Septal Perforation Repair - June 25, 2014
- Dr. Mantle recognized at the Beverly Hills Medical Science Academy Awards - May 8, 2014
- Commonly Misdiagnosed Pathologies: Arteriovenous Malformations - April 9, 2014
I’ve had a large squamous cell cancer on my scalp. I would like it removed but I am also concerned about the defect. What should I do?
Case Study
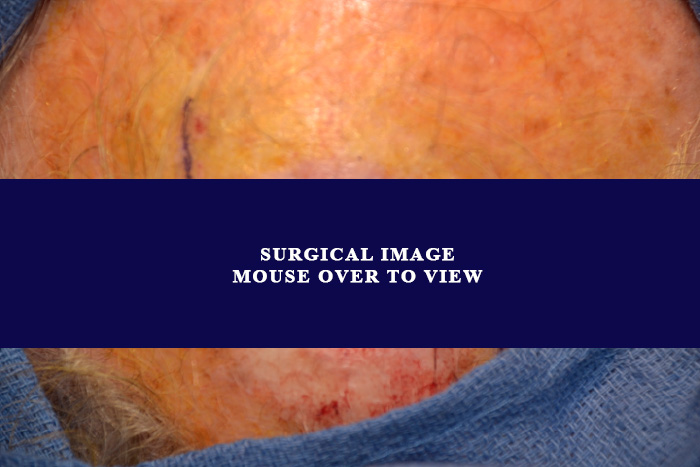
The patient is a 74-year-old male who noticed a crusting lesion of his scalp. This grew rapidly. A biopsy of the lesion was consistent with squamous cell carcinoma. He underwent excision of the lesion with wide margins. The resulting defect was measured to be 3 cm by 3 cm. The patient underwent reconstruction by Dr. Zandifar. He did have a prolonged post-operative healing time due to the size and the location of the defect. The incision was treated post-operatively with silicone and laser. On follow up, the patient had only a slightly visible scar.

Figure 1: Lesion before excision
Figure 2: Lesion after excision but before reconstruction

Figure 3: 6 months after reconstruction
Discussion
Skin cancers of the scalp are one of the hardest skin cancers to address. First, because most of the scalp is covered with hair the cancer is typically missed until it is larger in size. Second, the skin of the scalp is tight with little room to stretch and pull, making reconstruction a challenge.
It is not unlikely to need multiple procedures to fully reconstruct the scalp. In some cases, there may be a need for procedures such as tissue expander placements prior to reconstruction of the defect. This allows for stretching of the tissue around the defect and thus leads to extra skin being available for reconstruction. There is also increased need for post-operative care. Close wound care, use of topical treatments and lasers, and frequent follow-ups will usually lead to excellent cosmetic results. In almost all cases of scalp reconstruction, however, there is an increased post-operative healing time when compared to other locations on the face.
The physicians of the Osborne Head and Neck Institute are board certified in otolaryngology and plastic and reconstructive surgery. These surgeons carry a rare and complimentary subset of training specialties, allowing them to address not only the functional concerns of the nose but also the aesthetic implications of disease treatment.
To learn more about Dr. Hootan Zandifar or squamous cell carcinoma reconstruction, please visit: www.ohniskin.com.