- Surgery and Your Voice - September 22, 2016
- Question: How do the ingredients in e-cigarettes and vaporizers affect respiratory health? - August 16, 2019
- Bad Technique and Vocal Injury - January 9, 2019
- Is Edible Marijuana Dangerous for the Voice? Myths Dispelled - December 18, 2018
- Surprise! You have a hemorrhage - January 31, 2018
- Graves’ Disease: Treatment Overview - September 25, 2017
- Adele and the Stigma of Vocal Injury - July 11, 2017
- Vocal Curbside Consult: How does the thyroid affect the voice? - May 16, 2017
- Vocal Curbside Consult: How do hormones affect the voice? - May 3, 2017
- Vocal Curbside Consult: How do emotion and stress affect the voice? - April 17, 2017
- Vocal Curbside Consult: Vocal Recovery After Illness - April 7, 2017
A voice professional may need to undergo a surgical procedure to treat a condition unrelated to voice and vocal function. However, many surgeries have unexpected effects on the voice. When operations center around the head and neck, it is easy to make the correlation between the surgery and its potential impact on one’s voice. Less well-known are the effects that general surgical procedures and other seemingly unassociated operations can have on the voice. Almost all surgical procedures will have a direct or indirect effect on the voice. Consequently, it is important to consider voice-related side effects before undergoing any surgical procedure.
 How does general anesthesia affect the voice?
How does general anesthesia affect the voice?
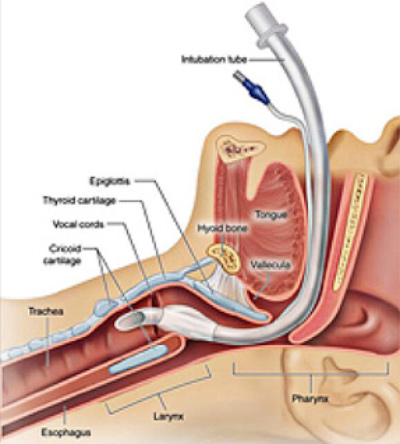
Many surgeries utilize general anesthesia, which may affect the vocal cords in the short term post-operative period. General anesthesia frequently requires endotracheal intubation, a procedure in which a breathing tube is placed between the vocal cords to regulate the patient’s breathing during surgery. Intubation can lead to hoarseness, throat pain, temporary loss of voice, and vocal cord swelling (edema). These symptoms may also appear if breathing is controlled by a less invasive laryngeal mask in lieu of intubation. While uncomfortable and irritating, these symptoms normally only persist for a few days. However, there is some risk of more permanent trauma, so patients should undergo a follow-up videostroboscopy examination with their laryngologist prior to resuming singing.
What are some common cosmetic head, face, and neck surgeries that might potentially affect the voice? How?
Patients considering facial plastic surgery should partner with their laryngologist to determine if and how a procedure can affect voice resonance. Rhinoplasty or a nose-job may result in narrowing of the nasal cavity, restricting airflow and changing the pitch and tone of the voice. This effect, known as hyponasality, results in increased nasal, high pitched, or congested sounds, similar to when you have a stuffy nose. Changes in resonance may also occur in facelift or neck lift procedures. While these vocal changes are not normally noticeable in everyday speech and conversation, the trained vocalist/listener may notice differences in tone, pitch, and range.
What are some common non-vocal invasive surgeries pertaining to the head, face, and neck that might potentially affect the voice? How?
Sinusitis/Sinus Infection: Sinuses affect the resonance of the voice, so sinusitis can be a big problem for vocalists. While some cases of chronic sinusitis can be treated with medication such as a nasal spray, severe cases of sinusitis may require sinus surgery. This surgical procedure treats the cause of sinusitis (lack of proper fluid drainage) by widening the sinus openings, in hopes of warding off any further infections. Widening these passages may cause changes in the voice, and is an important factor when considering sinus surgery.
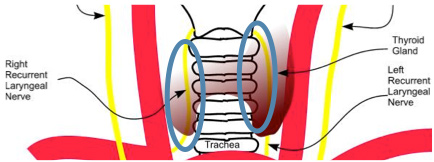
Thyroid Surgery: The thyroid is very close to the laryngeal nerves that supply the vocal folds. Consequently, surgical procedures in this area can potentially lead to nerve damage. Damage to these nerves can lead to loss of range, breathiness, or permanent hoarseness.
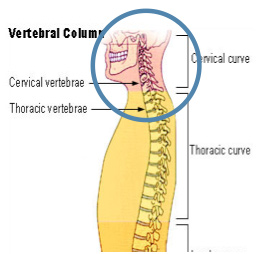
Cervical Spine Surgery: When operating on the cervical section of the spine (the end closest to the neck), some procedures access the spine from the front of the neck. This approach requires the surgeon to move and put traction on the laryngeal nerves in order to gain access to the spine. For this reason, some spine surgeons collaborate with a head and neck surgeon to ensure safe access to the spine. In either case, some studies report vocal weakness at rates as high as 11% though it is likely underdiagnosed when symptoms are subtle.
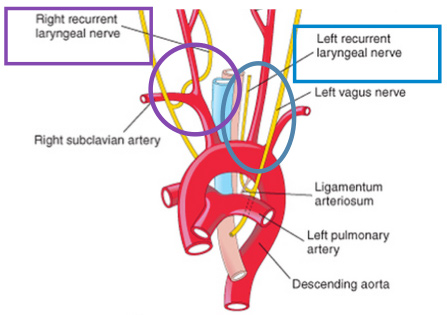
Cardiac Surgery: Heart surgery can affect the laryngeal nerves as well. The right recurrent laryngeal nerve winds through a prominent artery and the left laryngeal nerve hooks underneath the aorta, which is the main artery in the body. During cardiac surgery, the laryngeal nerves can be damaged, especially on the left side, resulting in nerve paralysis. This happens most commonly in surgeries that focus on the aorta, such as thoracic aortic aneurysm repair, though any type of cardiac surgery can result in voice damage.
How can you prevent this from happening to you?
The number one step in making sure your surgery won’t harm your voice is to consult with a qualified and experienced laryngologist to learn about any possible vocal side effects of a particular procedure. This will give you a better understanding of the risks involved with your surgery, and allow you to work with your surgeon to minimize those risks.
To learn more about the effects of surgery on the voice, please visit: www.ohni.org.



