- Question: How do the ingredients in e-cigarettes and vaporizers affect respiratory health? - August 16, 2019
- Bad Technique and Vocal Injury - January 9, 2019
- Is Edible Marijuana Dangerous for the Voice? Myths Dispelled - December 18, 2018
- Surprise! You have a hemorrhage - January 31, 2018
- Graves’ Disease: Treatment Overview - September 25, 2017
- Adele and the Stigma of Vocal Injury - July 11, 2017
- Vocal Curbside Consult: How does the thyroid affect the voice? - May 16, 2017
- Vocal Curbside Consult: How do hormones affect the voice? - May 3, 2017
- Vocal Curbside Consult: How do emotion and stress affect the voice? - April 17, 2017
- Vocal Curbside Consult: Vocal Recovery After Illness - April 7, 2017
The patient is a 34 year old female who has had a several month history of decreased range. She has lost 2-3 notes off the top of her vocal range. This has occurred gradually but she is currently unable to access her upper range. Her history is only significant for a motor vehicle accident around the time of onset, but evaluation at that time did not demonstrate any vocal injury. Other symptoms include vocal fatigue and mild neck discomfort in the anterior neck.
Based on her history, we elected to do a flexible laryngoscopy. The exam is as follows:
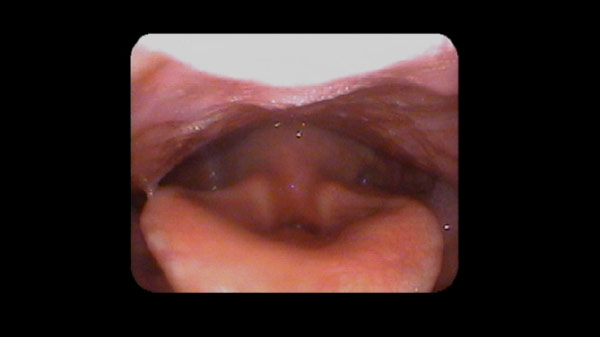

The video has several significant points, outlined in the timeline here:
0:00-0:19: Passage of endoscope through the nasal cavity
0:19-0:22: Simple task testing showing MTD
0:22-0:25: Freeze frame showing MTD – significant compression exists where vocal folds are obliterated from view.
0:36-0:46: Singing tasks shows a more open vocal tract
0:46-0:48: The patient listens to the vocal scale that she will attempt
0:48-end: Patient attempts with significant tension. At 0:53, there is near total collapse of the vocal tract
The patient’s diagnosis is muscle tension dysphonia (MTD). MTD is characterized by excessive use of compensatory vocal muscles, including pharyngeal muscles and false vocal folds. MTD patterns often develop in response to a change in the true vocal folds or the supporting musculature of the throat or neck. In this patient’s case, it is likely that the accident in which she was involved triggered compensatory muscle use patterns. After a period of time, these patterns become very difficult to reverse and become more firmly entrenched. Within 2 sessions of vocal therapy by a qualified vocal pathologist, this patient’s symptoms improved. Vocal range improvement and access will occur with her voice teacher.



