- Question: How do the ingredients in e-cigarettes and vaporizers affect respiratory health? - August 16, 2019
- Bad Technique and Vocal Injury - January 9, 2019
- Is Edible Marijuana Dangerous for the Voice? Myths Dispelled - December 18, 2018
- Surprise! You have a hemorrhage - January 31, 2018
- Graves’ Disease: Treatment Overview - September 25, 2017
- Adele and the Stigma of Vocal Injury - July 11, 2017
- Vocal Curbside Consult: How does the thyroid affect the voice? - May 16, 2017
- Vocal Curbside Consult: How do hormones affect the voice? - May 3, 2017
- Vocal Curbside Consult: How do emotion and stress affect the voice? - April 17, 2017
- Vocal Curbside Consult: Vocal Recovery After Illness - April 7, 2017
The patient is a 26 year old professional singer who noted an increase in vocal rasp and a decrease in vocal range over a 6-month period. She was performing more than usual during this 6-month period and noted that her symptoms were worse due to the increased voice use. She saw another laryngologist and was told that she had vocal fold nodules. She was referred for voice therapy, but did not have any notable improvement. The patient followed up and was told that she would need surgery because voice therapy failed to resolve her symptoms. She presented to the Osborne Head and Neck Institute, for a second opinion prior to proceeding with surgery.
At the time of presentation, the patient had an 11-note range. She was unable to produce sound above or below this range without becoming louder or forceful.
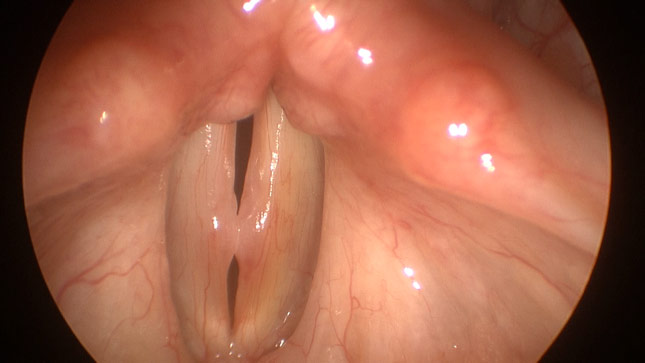
Her videostroboscopy is as follows:
The bilateral striking zones (middle third) of the vocal folds demonstrate significant thickening. There is stiffness and a lack of vibration in the striking zone, as well as a significant increase in erythema (redness) surrounding the nodules, suggesting ongoing trauma.
Although the patient was in the middle of a very busy schedule (gigs, recording, etc), voice therapy was prescribed with an understanding that it would take some time to be effective. While the patient continued to perform, she was advised to not record until the completion of her therapy. Successful voice therapy was expected to result in a significant improvement in voice quality.
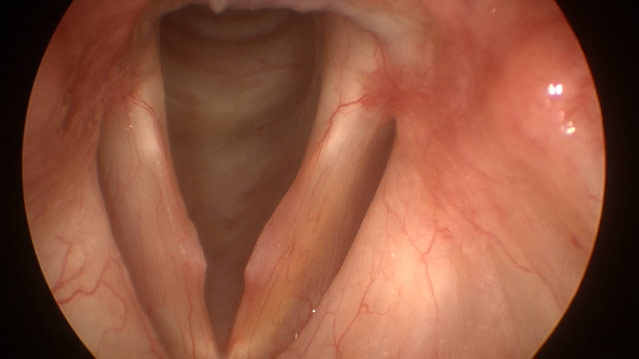
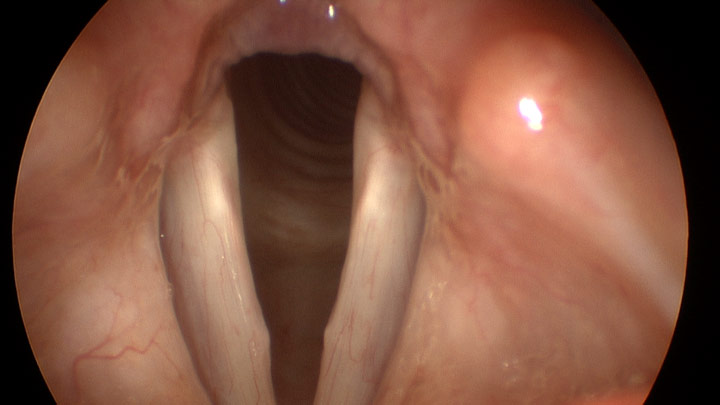
After 2 months of therapy, stroboscopy imaging demonstrated significant improvement.
The redness resolved, as did the nodular thickening. Although there is still minimal striking zone fullness, there is impressive improvement and resolution of vocal symptoms. The mild residual fullness should resolve.
Nodules are a reversible injury and should not require surgery, as has been previously discussed. Therapy will result in resolution, but does require some time to work. Even though the patient felt anxious about the time that was needed to resolve her problem, it is critical to reinforce that we are not treating a disease, we are treating a lifestyle.
Nodules occur in the setting of voice misuse and without correcting that behavior, they will persist or recur. Patients get into trouble when they rush into surgery due to their own scheduling constraints or the failure of conservative measures (i.e. poor voice therapy). Voice therapy is a very specialized skill that few speech pathologists do effectively. Simply having “done therapy” is not a reason to rush into surgery. When proper therapy is completed, those who have failed voice therapy may still find significant gains, as was seen with this patient. These results are only possible with a highly compliant patient.
It is critical to understand that surgical excision is not the answer it is often billed to be. Recurrence is very common and the attendant risks, including vocal scarring and loss of vocal range, are permanent. There is a role for surgery but it must be used judiciously and only upon failure of appropriate conservative treatments.
To learn more about Dr. Reena Gupta or nodules and voice therapy, please visit www.voicedoctorla.com.



